As the Covid-19 pandemic continues to impact resource allocation and professional experience across the spectrum of healthcare, we are learning more about how the novel coronavirus impacts cardiovascular health. We’ve also got more insight into the restructuring of practice — cardiology during COVID-19.
This Quality Matters news brief explores new developments surrounding the cardiovascular impact of SARS-CoV-2. Specifically, we look at how the virus impacts cardiovascular function in patients, some potential treatments to minimize the cardiovascular risk of what many initially considered to be a singularly respiratory virus, and the lasting effects on cardiovascular systems of care that the pandemic might leave in its wake.
Coronavirus May be a Blood Vessel Disease, Which Explains Everything – Elemental (by Medium)
Understanding this new disease’s impacts on cardiovascular health is crucial when examining and evaluating cardiology during COVID-19. Looking past the slightly clickbait-y claim that understanding the SARS-CoV-2 virus primarily as a blood vessel disease “explains everything,” this article does a great job of sketching out the cardiovascular impact of the novel coronavirus, and suggesting potential treatment strategies that extend beyond antiviral approaches which have been the primary focus thus far. As William Li, MD (President, The Angiogenesis Foundation) points out, SARS-CoV-2 carries a host of “seemingly unconnected phenomena that [we] do not normally see with SARS or H1N1 or, frankly, most infectious diseases.”
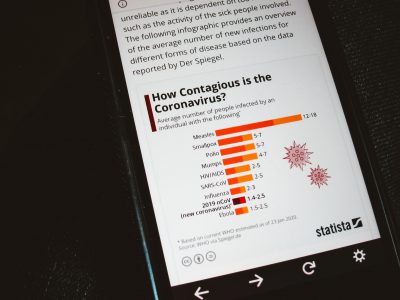
Around 40% of Covid-19-related deaths can be tied back to cardiovascular complications, and we know now that it is as much a vasculotropic virus as a respiratory virus. SARS-CoV-2 has a significant detrimental impact on endothelial cells, and while there are other diseases which have been known to impact endothelial cells, such as Ebola and Dengue, the etiologies of these two diseases is quite different from SARS-CoV-2, making generalizing information from them difficult.
Benhur Lee, MD (microbiology professor, Icahn School of Medicine at Mount Sinai) has suggested that the key difference between the original SARS virus and the SARS-CoV-2 virus is the protein required to spread the active virus throughout the body after the virus has attached to ACE2 receptors. Where the protein required to “crack open” the original SARS virus can only be found in the lungs, the novel coronavirus can be activated and spread by a protein – furin – found in all cells throughout the body, especially in the endothelium. “It’s ubiquitous,” said Lee.
As a result of these additional complications in treating SARS-CoV-2, many have begun to look for alternative treatments that extend beyond the frequently inadequate mechanical ventilatory support. In a “paper that looked at nearly 9,000 people with Covid-19, [Mandeep Mehra, MD, Medical Director of the Brigham and Women’s Hospital Heart and Vascular Center] showed that the use of statins and ACE inhibitors were linked to higher rates of survival.” Some are now speculating that stabilizing vascular endothelial may be an alternative to antiviral therapy in Covid-19, which may reduce mortality.
Blood Test May Predict Clot Risk in Severe COVID-19 – MedPage Today
Given the growing body of evidence surrounding the risk of clotting in patients with Covid-19, many clinicians are looking for new ways to quickly identify which Covid-19 patients are at the highest risk for thrombotic events, as stroke and/or heart attack are increasingly being linked to Covid-19. This article explores the results of a single-center study at Baylor St. Luke’s Medical Center ICU, which explored thromboelastography (TEG) as a predictor of thrombotic events.
Hypercoagulable TEG parameters were found to be more effective predictors than other coagulation markers (prothrombin time, INR, partial thromboplastin time, and platelet levels), and were associated with the development of clinically significant thrombosis in 13 of 21 PCR-test-positive patients. “[This] subclinical hypercoagulation microthrombosis syndrome is a very under-considered, underrecognized element of mortality risk” in COVID-19 said, Todd Rosengart (Professor & Chair Dept. of Surgery, Baylor College of Medicine). This may refocus clinical attention away from ventilation, pulmonary, and sepsis management, which have received a great deal of attention thus far as clinicians contend with the novel coronavirus.
Rosengart went on to suggest that all patients with severe cases of Covid-19 should “get TEG, and the patients who have abnormal TEG” should be treated with intravenous heparin, which has been a suggested treatment for persistent Covid-19-related clotting. The article goes on to stress the truly iterative nature of Covid-19 treatment at the moment, as there is still much we do not know, and cautions against any “dogmatic” views of treatment.
Restructuring Structural Heart Disease Practice During the Covid-19 Pandemic – JACC
Do we need to fundamentally restructure cardiology during COVID-19? Departing slightly from the precise etiology of Covid-19 in regard to cardiovascular function, this article provides recommendations for structural heart disease clinical pathways during the Covid-19 pandemic. Looking at the available international data surrounding the impact of Covid-19 on heart function, and considering the experience of a high-volume heart team in New York, JACC has generated these “reality-based considerations” in lieu of having access to “analytic outcomes data to guide evidence-based decision-making.”
These recommendations were compiled in an effort to ensure timely treatment while minimizing risk of exposure and limit the use of constrained resources. They are intended to be used to guide necessary adaptations to practice in the wake of local Covid-19 surges. Among the strategies and techniques discussed are the ongoing transition to telemedicine where possible, cancellation and reprioritization of structural heart procedures, patient selection measures which account for resource constraints, adaptations to the physical space and staffing of the cath lab/hybrid OR, and how to appropriately stage healthcare’s return to normalcy.
This guideline document, while largely speculative due to the lack of analytical data at our disposal, suggests that “this pandemic is likely to have a long ‘tail,’ and adjustments to usual practice will be necessary well into the foreseeable future.” These adjustments include considerations such as continued social distancing measures, and the use of PPE as a standard part of structural heart procedures. Additionally, the communication protocols between healthcare providers and patients are likely to see sustained changes after the pandemic has started to ebb. Expectation setting, patient education regarding self-monitoring, and transparency are going to be critical going forward, as patients begin to ease away from the caution that may make them hesitant to seek in-person care.
Acute coronary syndromes during COVID-19 – European Heart Journal
This short document proposes that all ACS patients should be considered potential carriers of the SARS-CoV-2 virus in order to ensure maximum safety precautions are taken for other patients and for hospital staff. One change in protocol that the document suggests is that, when bringing STEMI patients to the hospital, in addition to electrocardiogram (ECG) and clinical ACS information, ambulance crews should provide cardiologists “a detailed history of the patient’s possible contact with COVID-19 illness, and details of the presence of suspected symptoms within the last 14 days.”
The recommendations in the document also provide a four-category framework for patients post-ACS-triage, which outlines patient conditions (both known conditions and assumed conditions), and the necessary PPE/treatment protocol for each case.
Reductions in Heart Failure Hospitalizations During the COVID-19 Pandemic – Journal of Cardiac Failure
This letter to the editor seeks to accurately characterize “trends in urgent or emergent hospitalizations including heart failure (HF) hospitalizations,” which represent a gap in our knowledge of hospitalizations and procedures thus far in the Covid-19 pandemic. The authors note that after “the first case of COVID-19 was diagnosed in Mississippi, there was a sharp 50% decline in the number of HF hospitalizations that declined even further after a ‘state of emergency’ was declared.”
As the article points out, “most HF hospitalizations are non-elective and represent worsening congestion that can have significant impact on patient outcomes if not treated or delayed,” and hospital and/or health authority policies should not have impacted the total number of cases. The conclusion of the authors is that “patient fear of medical facilities” is responsible for this decline in HF cases, and that “further urgent attention to understand and mitigate these patterns” is needed including alternative patient monitoring, more frequent patient communications, and new therapeutic approaches to HF care. Patients still need quality cardiology during COVID-19!