While there are an abundance of resources advising caution when discussing new potential treatments for COVID-19—and rightly so—we’d like to take the opportunity to collect some positive perspective on the future as we close the book on the first six months of “the new normal.” That might require looking for some silver linings in the clouds of noise surrounding daily COVID-19 updates as well as some analysis of what’s gone wrong—which we can positively spin as showing us how to be better prepared for global health crises in the future. Perhaps it’s a tall order, but this Quality Matters is all about COVID-19 causes for optimism.
COVID-19 Drug Research is a Big Huge Mess – Wired Magazine
Okay, sure—this may not seem like the right headline to include in our covid-19 causes for optimism, but let’s jump right into what’s gone wrong and how we can improve our systems for better, faster science in the future. The Wired article calls out a “lack of coordination” for slow progress on our developing clinical protocols and science on treatment for patients with COVID-19. “Each hospital tried to develop their own protocol,” says Tracy Wang, MD, of Duke Clinical Research Institute. “Every hospital just launched its own variation on things. And at the end of the day, we couldn’t study this in a multi-center, large-scale fashion.”
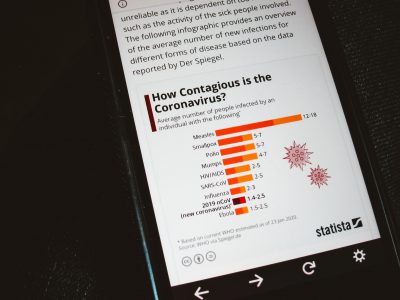
The article cites a research letter published July 27 in JAMA Internal Medicine in saying that of 1,551 COVID-19 studies entered into the US registry between March and May, only 10 percent were double-blinded and had more than 100 participants. “Less than 40 percent of all those trials would have the statistical power to conclude anything meaningful,” reads the article. “There aren’t that many studies that are going to move the needle in terms of generating evidence,” says Mintu Turakhia, MD of Stanford University who authored the research letter. Perhaps most damning in all of this, is that this seems to be status quo for how clinical research is done, in general. “We lack any sort of organized and systematic approach to testing therapeutic ideas,” says Peter Bach, director of the Center for Health Policy and Outcomes at Memorial Sloan Kettering Cancer Center. “I don’t know what to say other than it is always like this, really.”
To see the bright side in all of this is to say, well, at least the burning platform is illuminating and providing impetus for improving the way we conduct clinical science. “All of us agree there is an imperative to do this, and time is of the essence,” says Wang in the Wired article. “Now we just need to make the machine that makes this run a little faster. And I’m certain this machine will persist after the pandemic.” Read more »
Could an accreditation network be the answer?
Could a network of sites meeting the standards of a rigorous and supportive accreditation process provide this kind of scientific infrastructure? At Accreditation for Cardiovascular Excellence, good clinical science is core to our mission—and we believe our systems could help provide more coordinated scientific efforts on a global scale. Standards related to a site’s readiness to conduct clinical research could easily be incorporated or added-on as an additional distinction to our evidence-based standards. Achieving accreditation with this distinction would not only identify a global network of sites with the capacity to launch coordinated research, but also the value-added nature of the supportive accreditation process would signal sites’ commitment to coordinated clinical science and advancing quality care. Accreditation would further provide its usual third-party, non-biased benefits in ensuring site compliance and maintenance in an on-going capacity, and signalling to policymakers and funders an organization’s quality. We’re optimistic that accreditation can help systemically improve quality care in this way. What do YOU think? Should ACE be committed to building this scientific network infrastructure?
Low-Tech Way to Help Some Covid Patients: Flip Them Over – New York Times
Of course, that first article is not to say that we haven’t learned anything about treating COVID-19 in six months. In fact, we find a number of COVID-19 causes for optimism in this high-profile story from back in May. Firstly, that despite the dearth of large scale, coordinated scientific efforts, health professionals’ sincere and concentrated efforts regardless have led clinicians to have more potential tools in their toolbox in fighting the disease, including this low-tech one which may help even in cases where ventilator capacity is in question. This example is also particularly encouraging because it suggests a rapid uptake of competency in interdisciplinary non-physician teams at performing a maneuver which is not exactly easy or simple with many patients. “It’s a bit like going into battle,” said Dr. Michelle Ng Gong, MD, of the Montefiore Health System in New York. “The ability to turn these patients safely without dislodging a tube, without something accidentally falling out, without a patient going into cardiac arrest, that takes team coordination.” But observationally, we see a pattern playing out that is very familiar to clinicians in invasive cardiovascular care—the roll-out of new therapeutic innovations and techniques and the minimization of complications as volume increases. “There’s certainly a lot of anxiety about that when you talk about rolling out something if you haven’t done it a lot,” said Dr. C. Corey Hardin of Massachusetts General Hospital. But “once you’ve done it a couple of times, people are like, ‘Oh wow, this isn’t that big of a deal.’” The systemic improvement of care for ventilated patients, in general, thanks to this simple yet complex inter-disciplinary competency innovation is cause for optimism going forward. Read more »
Some (Modest) Good News on Covid-19: Doctors Are Getting Better at Treating It – Wall Street Journal
On a similar note, this article from July 31 does a good job of summarizing how far we’ve come in the six months that the world has been tackling severe COVID-19 cases—we better understand the disease’s pathophysiology and have more tools in our toolbox to combat it. “Crucially, doctors now know that Covid-19 isn’t just a respiratory disease but that it can potentially affect the cardiovascular and nervous systems, for instance,” reads the article. “The emerging approach focuses on treating a handful of frequently observed symptoms of severe Covid-19 that can turn deadly. First is delivering enough oxygen. Second is reducing the risk of blood clots. Third is tackling inflammation of the organs and tissues caused by a runaway immune response to the virus. Doctors say some patients also need treatment for kidney failure.” Plus, we have had some good, practical clinical science come from the UK’s “Recovery” trial which has found therapeutic benefit for dexamethasone in reducing deaths among very sick patients. Read more »
When will we get COVID-19 vaccine? Fauci ‘cautiously optimistic’ about this timeline – Miami Herald
Plus, among the COVID-19 causes for optimism are the dozens of vaccines in accelerated tests as well as novel antiviral medications that are entering phase three trial testing. Even Dr. Anthony Fauci, who might be best known for reminding the public to be cautious about any unproven treatments—including skepticism about Russia’s reported vaccine to be rolled out—says he’s “cautiously optimistic” about a timeline for an effective vaccine to be identified by late Fall or early Winter. Read more »
Fighting COVID-19 by luring the virus away from human cells with a decoy target – Fierce Biotech
And finally among our COVID-19 causes for optimism: while reputable and considerate medical news sources have been careful to tout recent, promising results of potential treatments tested at a cellular level—not in clinical trials—they are certainly cause for optimism. This article from Fierce Biotech does a good job of describing the core innovation of several studies’ findings without being overly optimistic about the many wondrous uses of seaweed extract or any particular treatment. “A soluble high-affinity ACE2 variant could offer one advantage in the resistance wars: To escape neutralization, the virus would have to mutate in a way that decreases its ability to bind with human cells’ native ACE2 receptors,” reads the article. “And that, in turn, would make it less infectious, Erik Procko, the study’s senior author, explained in a statement.” The article also describes how a separate team has found cellular efficacy of the blood thinner heparin acting in a similar fashion as a “decoy.” Read more »