Is your facility making any of these common cath lab mistakes? Original science (2019) from Accreditation for Cardiovascular Excellence (ACE) identifies 11 specific domains where most cath labs under review only partially met or did not meet ACE quality standards to help target quality improvement efforts, broadly, with tips on how to achieve quality improvement gains. These findings are reviewed in the context of ACE’s newly updated 2020 Cath/PCI standards with one NEW area for the focus of timely quality improvement efforts in your organization.
ACE Standards Focus Quality Improvement
Two weeks ago, we announced the release of our newly updated, openly available 2020 standards for the cardiac catheterization laboratory, and last week we did a deeper dive into how those standards were developed and what’s notable and new in the document.
But as our quality standards are geared towards focusing quality improvement efforts—the standards “set a bar that facilities can use to compare themselves to,” says ACE’s Chief Medical Officer, Bonnie Weiner, MD, MBA—we also wanted to take an opportunity to review all of the standards for those domains and areas where organizations most commonly demonstrate shortcomings upon comprehensive accreditation review.
In our recent award-winning poster from the American College of Cardiology’s 2019 Quality Summit, we reviewed quantitative and qualitative data from 14 accreditation reviews to identify those domains where facilities most commonly fell short of meeting ACE quality standards, finding 11 domains and 5 common areas for improvement. We add a 6th area to that original list, reflective of our new Cardiogenic Shock standards which facilities should ensure they have integrated into their procedures and protocols.
11 Common Cath Lab Mistakes
1. Not having a protocol to follow-up on patients at high-risk for contrast-induced nephropathy.
A follow-up on renal function in patients at high risk (i.e. GFR <60) for nephropathy is a must-have to ensure patient safety and quality care in the cath lab, due to an increased risk of contrast-induced nephropathy during Cath/PCI procedures. In our review, 12 out of 14 organizations did not meet this standard—having no set protocols or procedures for following up with these patients. Does your organization follow-up on patient renal function?
2. Not consistently managing patients at high-risk of nephropathy during procedures.
Distinct from number one, it’s also important for organizations to pay special attention to these high-risk patients in preparing them for PCI and managing them following the procedure. Pre- and post-procedure hydration, for example, is important in minimizing contrast-induced nephropathy risk, and facilities should have specific protocols and procedures to ensure this takes place. While a majority of organizations partially met this standard, it was still flagged as a shortcoming for all 14 reviewed facilities. Does your organization have a set protocol for managing these patients?
3. Not following up on fluoroscopy doses that exceed 60 minutes.
Post-procedure follow-up also results in our third common cath lab mistake, where reviewed organizations did not set protocols and procedures for surveilling and following up with patients for whom the recorded total air kerma at the interventional reference point (Ka,r,) is 5 Gy or greater, Pka of 500 Gycm2, or whom received fluoroscopy for more than 60 minutes. Due to potential adverse effects of cumulative radiation dose, these instances should be carefully recorded and justified, and the patients should be made aware of the risks. Does your facility follow-up on patient radiation exposure?
4. Not assessing diagnostic accuracy and adequacy via random case reviews.
A major shortcoming in ten out of fourteen facilities, this domain relates to the need for a sophisticated, randomized method of quality review of procedures, themselves, being assessed during an organization’s quality assurance process. This randomized case review of diagnostic accuracy is crucial to quality assessment and improvement in the cath lab. Does your facility do randomized case reviews?
5. Not using a peer-review process for indications and periodic review of all major complications.
Another common cath lab mistake related to quality assurance systems—organizations should have a system of peer-review of cases and their indications and periodically review all major complications. This is a crucial, core methodology for quality assurance and quality improvement. Does your facility have a sophisticated peer-review quality assurance system?
6. Not including comprehensive indicators and assessments in the process QA.
While the vast majority of reviewed facilities partially met standards related to the comprehensiveness of indicators and assessments in the facility’s quality assurance protocols, very few reached the level of comprehensiveness required by the latest scientific consensus and ACE standards for assuring and promoting quality care. These process indicators include: a) quality of angiographic studies, b) completion of accurate and informative reports, c) emergency response times, d) total procedure and fluoroscopy times, e) contrast usage, f) radiation dose, and g) other criteria. The required assessments include: a) the rate of non-obstructive coronary artery disease based on the NCDR CathPCI registry definition b) an assessment of MACCE and vascular complication rates for all types of procedures performed, and c) an assessment of the diagnostic accuracy and adequacy of angiograms. How comprehensive is your QA?
7. Inconsistently following Appropriate Use Criteria.
Appropriate Use Criteria reflect the scientific quality consensus on indications for cath lab procedures, but many facilities only partially meet ACE Standards with regards to their consistent use. Indications for all procedures should be consistent with published clinical guidelines to ensure quality, effective care. How well do you follow the AUC?
8. Not standardizing orders for the anti-coagulated patient undergoing cath procedures.
Facilities should have a written protocol or standardized order set for the anti-coagulated patient undergoing cardiac catheterization procedures and for various access site management including anticipating complications. Not properly anticipating or standardizing the response to more common complications leaves room for error in high pressure situations, and could have a significant adverse effect on complications. Is your response standardized for these patients?
9. No follow-up on physicians maintaining certifications and continuing ed. requirements.
Perhaps surprisingly, we found that eight out of fourteen reviewed facilities demonstrated shortcomings on standards related to physician ACLS certification, following facility standards for radiation safety, and obtaining 30 hours of Category 1 continuing medical education credits specific to invasive cardiology over a 2-year period. These indicators ensure that operators are maintaining up-to-date scientific knowledge on quality cardiac care while also maintaining core skills, and they are a prerequisite to a quality-leading cath lab team. Are your docs all keeping up?
10. No volume requirements for operators.
Science consistently shows volume requirements to be a major predictor of outcomes and quality in the cath lab, so organizations should have rules and metrics for ensuring individual operators meet and maintain requirements concordant with the most current ACCF/AHA/SCAI consensus competency document. Unfortunately, we found nine out of fourteen organizations to have short-comings on this point, not explicitly requiring a minimum recommended annual volume to ensure individual operator proficiency. Does your cath lab have volume requirements for operators?
11. Not documenting comprehensively.
Last but certainly not least is a topic that deserves its own article—documentation as a category featured the most instances of organizations not meeting ACE standards or only partially meeting ACE standards for the comprehensiveness of documentation, with more than double the instances of shortcomings across the fourteen reviewed organizations compared to any other category. In other words, of all the common cath lab mistakes, this one is by far the most common!
Comprehensive documentation is crucially important in quality assurance and quality improvement, as we cannot improve on what we do not accurately and completely measure.
While the official 2020 ACE Cath/PCI Standards have extensive details on documentation required, I’ll leave you with one specific standard that does a good job of encapsulating the importance of timely, accurate and comprehensive documentation. “Standard 8.1.2: There must be enough information in the record immediately after the procedure to manage the patient throughout the post-procedure period.”
5 Areas for Cath Lab Quality Improvement
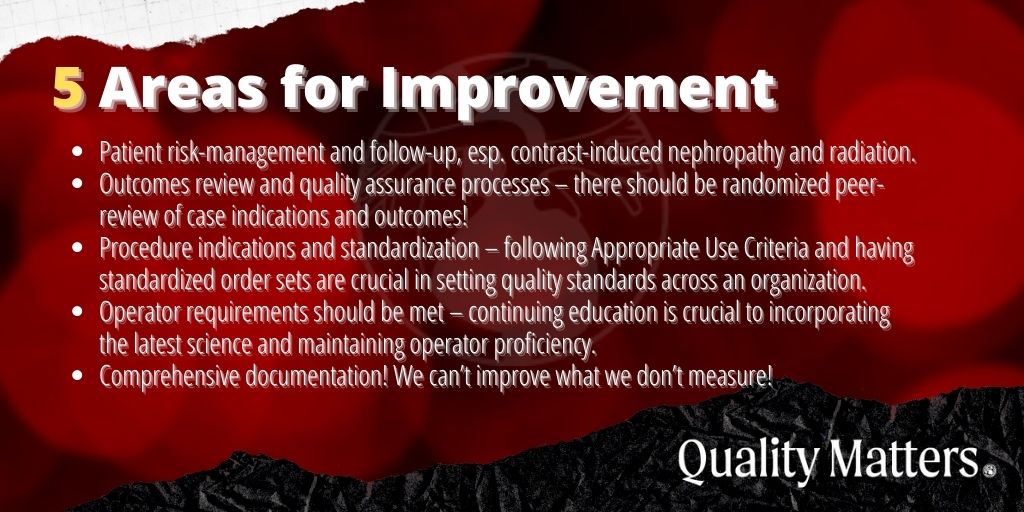
In summary, here’s a breakdown of five areas for cath lab quality improvement encapsulated in the 11 common cath lab mistakes, above:
- Patient risk-management and follow-up, especially contrast-induced nephropathy, patients on anti-coagulation, and radiation exposure.
- Outcomes review and quality assurance processes – there should be randomized peer-review of case indications and outcomes!
- Procedure indications and standardization – following Appropriate Use Criteria and having standardized order sets are crucial in setting quality standards.
- Operator requirements should be met – continuing education is crucial to incorporating the latest science and maintaining operator proficiency.
- Comprehensive documentation! We can’t improve what we don’t measure!
Bonus area: has your organization integrated the latest clinical consensus on Cardiogenic Shock into your protocols and procedures? A major component of our 2020 Cath/PCI Standards update is the inclusion of new section 7 on Cardiogenic Shock, developed in accordance with the SCAI Clinical Expert Consensus Statement on Cardiogenic Shock published in 2019.












